“I had COVID three months ago, but I still get winded walking up stairs,” my patient told me during our follow-up consultation. “Will my lungs ever be normal again?”
Long COVID affects millions of people worldwide, with respiratory symptoms among the most persistent and concerning complications. Understanding why lungs remain affected helps set realistic recovery expectations.
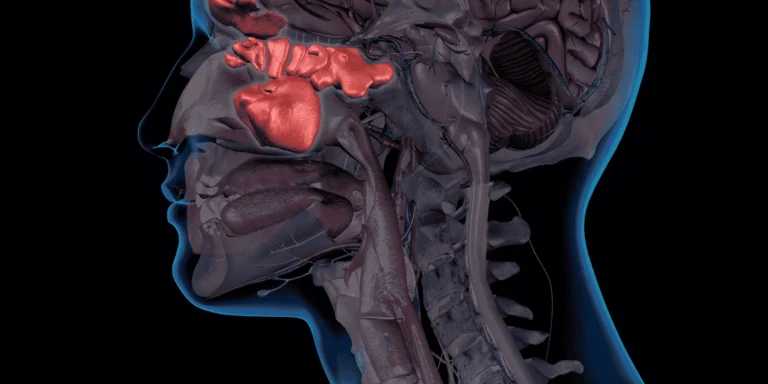
How COVID Damages Lung Tissue
Direct viral invasion occurs when SARS-CoV-2 virus attacks cells lining the airways and air sacs, causing inflammation and tissue damage.
Inflammatory response continues even after the virus clears, as the immune system keeps attacking lung tissues in some people.
Scar tissue formation can develop in areas of severe inflammation, creating permanent changes that affect breathing capacity.
Blood vessel damage in the lungs impairs oxygen exchange and can cause ongoing circulation problems.
Types of Persistent Lung Problems
Shortness of breath remains the most common long-term symptom, affecting daily activities like climbing stairs or exercising.
Chronic cough can persist for months after initial infection, sometimes dry and sometimes productive.
Chest tightness creates feelings of pressure or constriction that may worsen with activity or stress.
Exercise intolerance prevents people from returning to pre-COVID activity levels, with fatigue occurring much earlier than before.
Risk Factors for Long-Term Issues
Severe initial illness requiring hospitalization or oxygen support increases the likelihood of persistent lung problems.
Pre-existing lung conditions like asthma or COPD make people more vulnerable to lasting COVID effects.
Age over 50 correlates with higher rates of long-term respiratory complications.
Delayed medical treatment during initial infection may allow more extensive lung damage to occur.
Recovery Timeline Variations
Mild cases often see gradual improvement over 3-6 months, though some symptoms may persist longer.
Moderate cases typically require 6-12 months for significant improvement, with some people experiencing incomplete recovery.
Severe cases may have permanent lung changes that require ongoing medical management and pulmonary rehabilitation.
When to Seek Evaluation
Persistent symptoms lasting more than 8 weeks after COVID infection warrant pulmonary function testing.
Worsening breathlessness or new chest pain requires immediate medical evaluation to rule out complications.
Activity limitations that prevent normal daily functioning should be addressed with comprehensive respiratory assessment.
Diagnostic Approaches
Pulmonary function tests measure breathing capacity and identify specific areas of impairment.
Chest imaging can reveal scarring, inflammation, or other structural changes in lung tissue.
Exercise testing helps quantify functional limitations and guide rehabilitation efforts.
Blood oxygen monitoring identifies problems with oxygen exchange that may need treatment.
Treatment Options
Pulmonary rehabilitation programs help people regain lung function through supervised exercise and breathing techniques.
Anti-inflammatory medications may reduce ongoing inflammation that perpetuates lung problems.
Oxygen therapy becomes necessary for some people with severe oxygen exchange problems.
Bronchodilators can help open airways and improve breathing in people with persistent constriction.
Recovery Strategies
Gradual exercise progression helps rebuild lung capacity without overexertion that could worsen symptoms.
Breathing exercises taught by respiratory therapists can improve lung function and reduce shortness of breath.
Avoid irritants like smoke, strong chemicals, and air pollution that can worsen lung inflammation.
Long-Term Outlook
Most people improve over time, though recovery may take many months and may not be complete.
Younger, healthier individuals typically have better outcomes than older adults or those with chronic conditions.
Early intervention with appropriate treatments often leads to better long-term outcomes.
Research continues into new treatments that may help people with persistent COVID lung problems.
The key is recognizing that long COVID lung issues are real medical problems requiring appropriate evaluation and treatment, not simply “getting over” the initial infection.